Early Periodontal
Quick Answer
Periodontal disease typically begins with subtle warning signs including bleeding gums during brushing or flossing, persistent bad breath, and swollen or tender gums that appear reddish or purplish. If caught early in the gingivitis stage, gum disease is completely reversible with professional treatment and improved oral hygiene.
If your gums bleed when you brush, you might dismiss it as normal—but it’s actually one of the earliest warning signs your body sends when periodontal disease begins to develop. As a Chicago resident navigating the demands of work, family, and city life, paying attention to these subtle signals can mean the difference between a simple cleaning and more complex dental procedures down the road.
Nearly half of American adults over 30—approximately 47%—live with some form of periodontal disease, according to the Centers for Disease Control and Prevention. Yet many people in neighborhoods like Lincoln Park, Lakeview, and throughout Chicago don’t realize they have gum disease until it has already progressed to more serious stages.
Understanding the early signs of periodontal disease empowers you to take action before minor inflammation becomes a threat to your teeth and overall health.
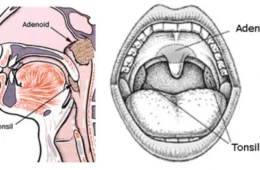
What Is Periodontal Disease?
Periodontal disease, commonly called gum disease, is an infection of the tissues that surround and support your teeth. The condition begins when bacteria-laden plaque—a sticky, colorless film—accumulates along the gumline and hardens into tartar.
Without proper removal through brushing, flossing, and professional cleanings, these bacteria trigger an inflammatory response in your gum tissue. What starts as mild inflammation can eventually destroy the soft tissue and bone that hold your teeth in place, potentially leading to tooth loss.
The disease progresses through distinct stages, each with different implications for treatment and your long-term oral health. The good news? When detected early, periodontal disease can often be reversed before permanent damage occurs.
The 7 Early Warning Signs of Periodontal Disease
Recognizing the early signs of periodontal disease is crucial for preventing progression. Many patients in our Chicago practice describe these symptoms as “barely noticeable” at first—which is exactly why regular dental checkups are so important.
1. Bleeding Gums During Brushing or Flossing
Healthy gums should never bleed. If you notice pink-tinged toothpaste when you spit or blood on your floss, this is your body’s first alarm bell.
While occasional bleeding might result from brushing too hard, consistent bleeding—especially with gentle pressure—indicates gum inflammation. This symptom appears in the earliest stage called gingivitis, when the infection hasn’t yet reached the bone.
2. Red, Swollen, or Puffy Gums
Healthy gum tissue appears pale pink and feels firm to the touch. When periodontal disease develops, gums become engorged with blood as your body attempts to fight the bacterial infection.
Chicago patients often describe their gums as feeling “tender” or “sore,” particularly around the areas where teeth meet gums. The tissue may take on a reddish or purplish hue rather than its normal light pink color.
3. Persistent Bad Breath (Halitosis)
Bad breath that doesn’t go away after brushing, flossing, or using mouthwash often signals bacterial overgrowth beneath the gumline. These bacteria release sulfur compounds that create an unpleasant odor.
If you’ve noticed others stepping back during conversations or you’re constantly reaching for mints, this chronic bad breath—medically termed halitosis—deserves professional evaluation.
4. Tender or Sensitive Gums
While early periodontal disease is typically painless, many patients notice increased sensitivity in their gum tissue. You might feel discomfort when eating hot or cold foods, or notice tenderness when you touch your gums.
This sensitivity occurs because inflamed gum tissue becomes more reactive to stimuli. Some Chicago patients in our practice report that even the pressure from their electric toothbrush feels uncomfortable on certain areas.
5. Gum Recession (Teeth Looking Longer)
When gums begin pulling away from teeth, more of the tooth surface becomes visible. You might notice this gradually—perhaps commenting that your teeth “look different” than they used to.
Gum recession doesn’t happen overnight. The process occurs slowly as inflammation causes the gum tissue to separate from teeth, creating small pockets where bacteria can accumulate. These pockets become breeding grounds for infection as your toothbrush and floss can’t reach them effectively.
6. Changes in Your Bite or Tooth Alignment
As periodontal disease progresses and affects the supporting bone, you might notice subtle changes in how your teeth fit together when you bite down. Some patients report that their partial dentures no longer fit as comfortably as they once did.
While this symptom typically appears in more advanced stages, paying attention to any changes in your bite can help catch the disease before significant bone loss occurs.
7. Plaque and Tartar Buildup Along the Gumline
A yellowish or brownish layer that forms along your gumline signals plaque buildup that has hardened into tartar (also called calculus). Unlike soft plaque that you can remove with brushing, tartar firmly adheres to teeth and can only be removed through professional cleaning.
This visible buildup provides the perfect environment for bacteria to thrive and multiply, accelerating gum disease progression.
Early Signs vs. Advanced Signs of Periodontal Disease
| Category | Early Signs (Gingivitis / Early Periodontitis) | Advanced Signs (Moderate to Severe Periodontitis) |
|---|---|---|
| Gum Appearance | Red, swollen, or slightly puffy gums | Deep gum recession, gums pulling far from teeth |
| Bleeding | Bleeding during brushing or flossing | Spontaneous bleeding, even without brushing |
| Breath / Taste | Persistent bad breath (halitosis) | Strong foul odor, bad taste from pus or infection |
| Pain / Sensitivity | Mild tenderness or sensitivity | Pain when chewing, sharp sensitivity from exposed roots |
| Tartar / Plaque | Visible buildup along gumline | Thick tartar deposits extending under gums |
| Periodontal Pockets | 3–5mm pocket depth | 6–10mm pockets with severe tissue loss |
| Bone Loss | Minimal or beginning bone loss | Significant bone loss visible on X-rays |
| Tooth Stability | Teeth feel normal | Loose, shifting, or drifting teeth |
| Bite Changes | Rare at early stage | Noticeable changes in bite alignment, dentures not fitting |
| Gum Color | Reddish or purplish | Dark red, infected areas, or visible pus |
The Four Stages of Periodontal Disease
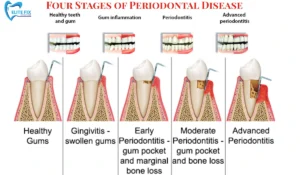
Stages of Periodontal Disease
Understanding how periodontal disease progresses helps explain why early detection matters so much for your long-term oral health.
Stage 1: Gingivitis (Reversible)
Gingivitis represents the mildest and only reversible stage of gum disease. At this point, inflammation affects only the gum tissue—the bone that supports your teeth remains undamaged.
Symptoms include:
- Red, swollen gums
- Bleeding during brushing or flossing
- Minor gum sensitivity
- Potential bad breath
Treatment: Professional dental cleaning combined with improved at-home oral hygiene can completely reverse gingivitis. Many of our Lincoln Park patients see dramatic improvement within just a few weeks of treatment.
Stage 2: Mild Periodontitis (Early Periodontal Disease)
Once bacteria penetrate beneath the gumline and begin attacking the bone, the disease enters periodontitis. This stage is no longer reversible, but it can be effectively managed with professional treatment.
Symptoms include:
- Gum recession (gums pulling away from teeth)
- Formation of periodontal pockets (spaces between teeth and gums measuring 4-5mm)
- Early bone loss visible on X-rays
- Continued bleeding and inflammation
Treatment: Scaling and root planing—a deep cleaning procedure performed under local anesthesia—removes bacteria from below the gumline and smooths root surfaces to help gums reattach.
Stage 3: Moderate Periodontitis
At this stage, the infection has spread deeper into the gum tissue and bone. The damage becomes more evident both visually and on dental X-rays.
Symptoms include:
- Deeper periodontal pockets (5-6mm)
- More pronounced gum recession
- Teeth may feel slightly loose
- Possible pus between teeth and gums
- Persistent bad breath despite good oral hygiene
- Increased tooth sensitivity
Treatment: More intensive interventions may be required, including more frequent deep cleanings, antibiotic therapy placed directly into periodontal pockets, and potentially pocket reduction surgery.
Stage 4: Advanced Periodontitis
The most severe stage involves significant bone and tissue loss. At this point, teeth may become so loose they need to be extracted.
Symptoms include:
- Severe gum recession
- Very deep pockets (7mm or greater)
- Shifting or loose teeth
- Pain when chewing
- Visible pus and infection
- Significant bad breath and bad taste
Treatment: Advanced periodontitis often requires surgical intervention, including bone grafts, gum grafts, guided tissue regeneration, or tooth extraction followed by dental implants or dentures.
The American Academy of Periodontology provides an in-depth explanation of how gum disease progresses from gingivitis to advanced periodontitis.
Why Early Detection Matters: The Real Impact of Periodontal Disease
Catching gum disease in its earliest stages provides the best outcomes for both your oral health and your wallet. The difference between gingivitis treatment and advanced periodontitis can be substantial.
Financial Considerations
- Early-stage gingivitis: May require only routine cleanings ($100-200) and improved home care
- Mild to moderate periodontitis: Scaling and root planing typically costs $500-4,000 depending on severity
- Advanced periodontitis: Surgical treatments, grafts, and tooth replacement can exceed $10,000-30,000
Health Beyond Your Mouth
Research continues to reveal strong connections between periodontal disease and systemic health conditions. The bacteria and inflammation from gum disease don’t stay confined to your mouth—they can enter your bloodstream and affect your entire body.
Studies have linked periodontal disease to:
- Cardiovascular disease: Individuals with gum disease have a 19% increased risk of heart disease, rising to 44% in those over 65
- Diabetes complications: Type 2 diabetics with severe periodontitis face 3.2 times greater mortality risk compared to those with mild or no gum disease
- Respiratory infections: Bacteria from periodontal pockets can be aspirated into the lungs
- Pregnancy complications: Pregnant women with gum disease may face higher risks of preterm birth and low birth weight
- Dementia: Emerging research suggests potential links between chronic inflammation from gum disease and cognitive decline
Who’s at Higher Risk? Understanding Your Personal Risk Factors
While anyone can develop periodontal disease, certain factors increase your susceptibility. Understanding your risk profile helps you take proactive steps to protect your gum health.
Non-Modifiable Risk Factors
- Age: Prevalence increases with age; nearly 60% of adults 65 and older have some form of gum disease
- Genetics: Family history plays a significant role in how your immune system responds to oral bacteria
- Gender: Men develop periodontal disease more frequently than women (50.2% vs. lower rates in women)
Modifiable Risk Factors
- Smoking and tobacco use: Current smokers have a 62.4% prevalence of periodontitis—smokers are three times more likely to develop severe gum disease
- Poor oral hygiene: Inconsistent brushing and flossing allows plaque accumulation
- Diabetes: 60% of adults with diabetes also have periodontitis; the relationship is bidirectional
- Stress: High stress levels suppress immune function, making it harder to fight oral infections
- Medications: Certain drugs reduce saliva production or cause gum overgrowth
- Poor nutrition: Diets lacking vitamin C and other essential nutrients compromise gum health
- Obesity: Associated with increased inflammation throughout the body
Special Considerations for Chicago Residents
Living in Chicago presents unique factors that can affect your oral health. The city’s hard water may contribute to increased tartar formation. Cold winters often mean less attention to routine care—many patients postpone dental visits during harsh weather, allowing minor issues to progress.
Additionally, the stress of urban living, long commutes, and demanding work schedules common in Chicago can lead to delayed dental care and increased risk factors like stress and poor dietary choices.
How Dentists Diagnose Periodontal Disease
If you’re experiencing any early warning signs, your dentist will perform a comprehensive periodontal evaluation. Understanding what happens during this assessment can ease any anxiety about your appointment.
Medical and Dental History Review
Your dentist will ask about your overall health, medications, smoking habits, and any symptoms you’ve noticed. Be honest about your oral hygiene habits—this information helps create an accurate picture of your risk factors.
Visual Examination
The dentist inspects your gums for signs of inflammation, including:
- Color changes (healthy gums are pale pink; diseased gums appear red or purplish)
- Swelling or puffiness
- Bleeding
- Tartar accumulation
- Gum recession
Periodontal Probing
Using a thin, calibrated instrument called a periodontal probe, your dentist measures the depth of the space between your teeth and gums. This measurement is crucial for diagnosis:
- Healthy gums: 1-3mm pocket depth with no bleeding
- Gingivitis: 1-3mm with inflammation and bleeding
- Periodontitis: 4mm or greater indicates disease
Pockets deeper than 5mm often require more intensive treatment as they’re difficult to clean effectively even with professional care.
Dental X-Rays
Radiographs reveal bone loss that isn’t visible during the visual examination. These images help your dentist assess the severity of disease and track progression over time.
X-rays show the level of bone surrounding each tooth root. In healthy mouths, bone extends close to the crown of the tooth. As periodontitis progresses, bone loss creates a distinctive pattern on X-rays that helps guide treatment planning.
Treatment Options for Early Periodontal Disease
The earlier you seek treatment, the more conservative and effective your options will be. Here’s what you can expect based on the stage of disease.
Professional Dental Cleaning
For patients with gingivitis or very early signs of gum disease, a thorough professional cleaning may be sufficient. Your dental hygienist will:
- Remove all plaque and tartar from above the gumline
- Polish teeth to create smooth surfaces that resist plaque accumulation
- Provide personalized instruction on proper brushing and flossing techniques
Many Chicago patients are surprised by how much improvement they see from this simple intervention when combined with better home care.
Scaling and Root Planing (Deep Cleaning)
This non-surgical procedure is the gold standard for treating mild to moderate periodontitis. Often called “deep cleaning,” scaling and root planing involves:
Scaling: Removing plaque and tartar from above and below the gumline, reaching deep into periodontal pockets
Root planing: Smoothing the tooth root surfaces to remove bacterial toxins and create a clean surface where gums can reattach
The procedure is typically performed under local anesthesia to ensure your comfort. Depending on the extent of disease, treatment may be completed in one appointment or divided into multiple sessions.
Antibiotic Therapy
For pockets that don’t respond fully to scaling and root planing, your dentist may place antibiotic microspheres or gels directly into the periodontal pockets. This localized treatment targets stubborn bacteria with minimal systemic side effects.
Some cases may also benefit from oral antibiotics to help control bacterial infection throughout the mouth.
Antimicrobial Mouth Rinses
Prescription-strength antimicrobial rinses can help reduce bacteria in areas that are difficult to reach with brushing and flossing. These rinses serve as an adjunct to—not a replacement for—proper mechanical cleaning.
Research from the National Institute of Dental and Craniofacial Research highlights how periodontal disease contributes to systemic inflammation.
Prevention: Protecting Your Gums for Life
The most effective treatment for periodontal disease is preventing it from developing in the first place. These evidence-based strategies can significantly reduce your risk.
Daily Home Care Essentials
Brush twice daily for two minutes each time:
- Use a soft-bristled toothbrush or electric toothbrush
- Hold the brush at a 45-degree angle to the gumline
- Use gentle circular motions
- Don’t forget to brush your tongue, which harbors bacteria
Floss once daily:
- Take time to clean between every tooth
- Curve the floss into a C-shape around each tooth
- Gently slide it beneath the gumline
- Use a clean section of floss for each tooth
Consider additional tools:
- Interdental brushes for larger spaces between teeth
- Water flossers to supplement traditional flossing
- Antimicrobial mouth rinse (use as directed by your dentist)
Regular Professional Care
Schedule dental cleanings and exams at least twice yearly—or more frequently if you have risk factors for gum disease. These appointments allow early detection of problems and remove hardened tartar that you can’t eliminate at home.
Many Chicago patients with increased risk factors visit our office every three to four months for periodontal maintenance cleanings. This proactive approach helps keep gum disease under control.
Lifestyle Modifications
Quit smoking: Tobacco use is one of the most significant risk factors for periodontal disease. Smoking restricts blood flow to gums, impairs healing, and suppresses immune function. Chicago offers numerous smoking cessation programs through the city’s public health department.
Eat a nutrient-rich diet:
- Foods high in vitamin C support gum health (citrus fruits, berries, bell peppers)
- Calcium and vitamin D strengthen teeth and bones (dairy, leafy greens)
- Omega-3 fatty acids reduce inflammation (fatty fish, walnuts)
- Crunchy vegetables naturally clean teeth
Manage stress: Chronic stress weakens your immune system and increases inflammation. Consider stress-reduction techniques like meditation, exercise, or therapy.
Control chronic conditions: If you have diabetes, work closely with your medical provider to maintain optimal blood sugar levels. Well-controlled diabetes reduces your risk of developing severe periodontal disease.
Special Considerations: Periodontal Disease in Different Life Stages
Pregnancy and Hormonal Changes
Pregnancy causes hormonal fluctuations that can make gums more sensitive to plaque bacteria. Many pregnant women develop “pregnancy gingivitis” characterized by swollen, bleeding gums.
If you’re pregnant or planning to become pregnant, inform your dentist. Maintaining excellent gum health during pregnancy benefits both you and your baby, as periodontal disease has been linked to preterm birth and low birth weight.
Teenagers and Young Adults
While periodontal disease is most common in adults over 30, aggressive forms can develop in teenagers and young adults. Early-onset periodontitis progresses rapidly and requires prompt, intensive treatment.
Parents should watch for warning signs in their children, particularly if there’s a family history of gum disease.
Seniors
As we age, our risk of periodontal disease increases. Nearly 70% of adults over 65 have some form of gum disease. Seniors may face additional challenges including:
- Medications that cause dry mouth
- Difficulty maintaining proper oral hygiene due to arthritis or mobility issues
- Cognitive changes that affect daily routines
Family members of older Chicago residents should help ensure regular dental care continues as part of overall health maintenance.
When to See a Dentist: Don’t Wait for Pain
One of the most dangerous aspects of periodontal disease is that it’s often painless in early stages. Many patients don’t realize they have a problem until significant damage has occurred.
Schedule an appointment immediately if you notice:
- Any bleeding from gums, even if occasional
- Changes in gum color or texture
- Persistent bad breath
- Gum recession or teeth looking longer
- Loose teeth or changes in your bite
- Pus between teeth and gums
- Any mouth sores that don’t heal
Even without symptoms, see your dentist regularly:
- Every six months for routine exams and cleanings if you’re low-risk
- Every three to four months if you have gum disease or risk factors
- As recommended by your dental team based on your individual needs
Don’t let the demands of Chicago life—busy schedules, long work hours, or weather challenges—delay essential dental care. Early intervention provides the best outcomes and prevents more complex, expensive treatments later.
Frequently Asked Questions
Can periodontal disease be reversed?
Gingivitis, the earliest stage, can be completely reversed with professional cleaning and improved oral hygiene. Once the disease progresses to periodontitis (where bone loss occurs), it cannot be reversed but can be effectively managed and controlled. With proper treatment and maintenance, you can halt further damage and maintain stable gum health for life.
How long does it take for periodontal disease to develop?
The timeline varies greatly depending on individual factors. Gingivitis can develop within days to weeks of inadequate oral hygiene. Progression from gingivitis to periodontitis typically takes months to years, though aggressive forms can advance much more rapidly—particularly in young adults with genetic predisposition.
Does periodontal disease cause tooth loss?
Yes, periodontal disease is one of the leading causes of tooth loss in adults. As the disease destroys the bone and soft tissue supporting teeth, they become loose and may eventually fall out or require extraction. However, with early detection and proper treatment, tooth loss can usually be prevented.
Is periodontal disease contagious?
While the bacteria that cause periodontal disease can be transmitted through saliva (such as during kissing or sharing utensils), not everyone exposed will develop the disease. Your susceptibility depends on factors including your genetics, immune system, oral hygiene habits, and other risk factors. Good oral hygiene practices protect you regardless of bacterial exposure.
What’s the difference between gingivitis and periodontitis?
Gingivitis is inflammation limited to the gum tissue without bone involvement. It’s completely reversible. Periodontitis occurs when inflammation extends deeper, causing irreversible bone loss and damage to the structures supporting your teeth. Think of gingivitis as the warning stage—address it promptly to prevent progression to periodontitis.
How much does periodontal treatment cost in Chicago?
Costs vary based on the severity of disease and treatment needed. Routine cleanings typically cost $100-200. Scaling and root planing for mild to moderate periodontitis ranges from $500-4,000 depending on how many quadrants require treatment. Advanced cases requiring surgery, grafts, or tooth replacement can exceed $10,000. Many dental offices, including EliteFixDenture.com, offer payment plans to make treatment accessible.
Can I treat periodontal disease at home?
While excellent home care is essential, professional treatment is necessary once periodontal disease develops. You cannot remove tartar (calculus) at home—it requires professional instruments. However, your daily brushing and flossing play a critical role in preventing disease and supporting professional treatment.
Will my insurance cover periodontal treatment?
Most dental insurance plans cover preventive care (cleanings and exams) at 100%. Coverage for periodontal treatment varies but typically includes a portion of deep cleaning costs. More extensive surgical procedures may have different coverage levels. Check with your insurance provider about your specific benefits, or contact our office for assistance navigating insurance questions.
Why do my gums bleed even though I brush regularly?
Regular brushing doesn’t necessarily mean effective brushing. Bleeding usually indicates inflammation caused by bacterial plaque. You might be missing areas during brushing, using incorrect technique, or not flossing. Bleeding can also result from brushing too hard. Schedule an evaluation with your dentist to identify the cause and receive personalized instruction.
Taking Action: Your Next Steps
Recognizing the early signs of periodontal disease empowers you to protect your oral health before minor problems become major concerns. If you’ve noticed any warning signs—bleeding gums, bad breath, or changes in your gum tissue—don’t wait for the symptoms to worsen.
Chicago residents in neighborhoods throughout the city, from Lincoln Park to Lakeview and beyond, trust EliteFixDenture.com for comprehensive periodontal care. Our experienced team understands the challenges of maintaining oral health in a busy urban environment and provides personalized treatment plans designed around your needs and schedule.
Whether you’re due for a routine cleaning or concerned about symptoms of gum disease, we’re here to help you maintain a healthy, confident smile.
About the Expert
Reviewed by Dr. Aziz Liaquat, Implant Dentistry Specialist
Dr. Aziz Liaquat brings extensive expertise in treating periodontal disease and its consequences, including advanced implant dentistry for patients who have experienced tooth loss. With a commitment to preventive care and patient education, Dr. Liaquat helps Chicago residents understand and address gum disease before it threatens their oral health.
Disclaimer
This article is for informational purposes only and is not a substitute for professional dental advice, diagnosis, or treatment. Always seek the advice of your dentist or other qualified health provider with any questions you may have regarding a dental condition. Never disregard professional dental advice or delay seeking treatment because of information you read in this article.
Take the First Step Toward Healthier Gums
Ready to protect your smile from periodontal disease?
For expert dental care in Chicago, visit EliteFixDenture.com or call our office today to schedule your comprehensive periodontal evaluation. Early detection saves teeth—and your smile.